Is it Time to Re-think the Zurich Guidelines?
February 27, 2014 5 Comments

Zurich: Site of the 2012 Meeting which
developed the current Consensus Statement
on Concussion in Sport
Vienna, Prague, Zurich: I’ve often wondered why the Consensus Statements on Concussion are made in central European cities.
The ‘International Consensus Conference on Concussion in Sport’ has taken place successively in Vienna (2001), Prague (2004), Zurich (2008) and again in Zurich (2012). It’s looking like the timing is an Olympiad! And as for venue, I suggest Budapest should start lobbying for 2016…..
But today we won’t be answering the ‘why’ of venue or timing regarding these conferences. We’ll be looking at commentary on the output of the last Zurich meeting: the so-called “Zurich guidelines,” or the Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012.
An editorial in our new, March 2014 issue, is entitled: Time to Re-think the Zurich Guidelines? A Critique on the Consensus Statement on Concussion in Sport. Written by Drs. Neil Craton and Oliver Leslie of Legacy Sport Medicine in Winnipeg, Manitoba, Canada, the piece is a provocative deconstruction of the Zurich Guidelines.
The authors have contributed to CJSM in the past. Last year, the pair wrote Concussion: Purely a Brain Injury? and Dr. Craton has contributed several other pieces over the years. The pair are also educators at the University of Manitoba Primary Care Sports Medicine Fellowship. They are busy clinicians as well as writers and teachers, and Dr. Craton includes as his clients the players of the Winnipeg Blue Bombers of the Canadian Football League (CFL).
Concussion, as defined by Zurich, is a subset of traumatic brain injuries. The formal definition, with which many of you will be familiar, is “…a brain injury and is defined as a complex pathophysiological process affecting the brain, induced by biomechanical forces.”
The editorial authors state that the Zurich guidelines, while providing high sensitivity, lack sufficient specificity. Consequently, they argue that Zurich opens up the possibility that a host of other pathologies (e.g. cervical strain, cervicogenic headaches, benign positional vertigo, etc.) can be construed as concussions. And if understood that way, the potential ‘mis-diagnosis’ can lead to iatrogenic harm: either by initiating a cycle of ineffective treatments, or causing undue worry among patients and families regarding a perceived brain injury. They go so far as to write, “The inclusion criteria for a diagnosis of concussion as articulated by Zurich are absurd (my itals).”
They further note concerns with Zurich regarding: 1) management strategies that are not ‘evidence based’ and 2) rehabilitation goals that are not attainable. They take specific issue with the notion of cognitive rest, stating it is not ‘intuitively obvious’ and is not formally defined. They also criticize the requirement for achieving an ‘asymptomatic’ status prior to beginning a return to play progression, and they cite a study that notes the average uninjured person will not score a zero on the 22-item, Likert Post-concussion Symptom Scale (PCSS). And so, they implicitly argue, what endpoint are we seeking when we are treating a patient with concussion?
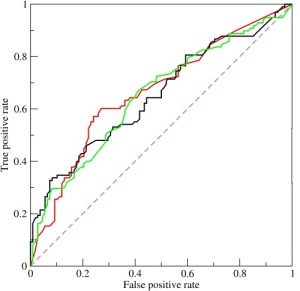
Sensitivity, Specificity: I wonder
what the ROC curve looks like
for the diagnosis of concussion
using Zurich guidelines?
It calls to mind the joke I make not infrequently in the room with patients and their families: as far as the PCSS goes, I think the last time I scored all zeros I was probably in my mother’s womb. Headache? Irritability? Drowsiness? Heck yes, if I’m late on my cup of coffee….
The authors make their strongest argument, I think, in what amounts to their peroration: they make an analogy between concussion and another ‘non-specific’ condition, fibromyalgia. “The medical community need only look to a non-specific condition like fibromyalgia,” they argue, “….to see the disability that can be promulgated by non-specific guidelines interfacing with patient hypervigilance, medical pseudoscience, legal wrangling and media scrutiny. We need a better way to protect the health of the athletes we serve.” That’s strong stuff, challenging. What do you think?
I encourage you to read the editorial, freely available, as I write, at our home page, and engage in the conversation that will surely ensue. The piece has already given me a great deal of food for thought. We’ll be talking more about it and related issues in the coming months, and we’re planning a podcast interview with the two authors. You won’t want to miss that!

This is an interesting item (and paper) – seems like debate about concussion definitions is still not over. But that is best left to clinicians to argue over, rather than to injury prevention folk like myself.
To me, with my interests in research knowledge translation and actual uptake of guidelines, I would like to see more emphasis on these implementation aspects. Whilst I fully accept the clinical ideals behind them, and the “gold standard” of clinical/medical assessment, there are so many times when this is impossible. For example, consider community-level (“weekend warrior”) sport played in rural areas (even in developed countries) or sporting competitions held in developing countries. In both cases, it is likely to be the cases that there is just not the medically-trained personnel available to treat/manage concussion. The guidelines stipulate that medical assessment before return-to-play is mandatory but this is often impossible. What should be done in these instances? Could there be a back-up, less ideal, but still acceptable approach to the management of concussion in these circumstances?
There are other issues around the implementation of the concussion guidelines – concerns shared by others not just me. Earlier this year, we published an expert appraisal of the 2008 statement (the precursor to the 2012 Zurich statement), available at:http://bjsm.bmj.com/content/48/2/130.abstract?sid=e117c684-a1c9-495e-bd77-cd6d8c4ffc81. This showed that a major criticisms of the earlier statement was a lack of implementation considerations, such as how to ensure their uptake. Many of these concerns .remain with the 2012 Zurich guidelines.
Perhaps, what is now needed to be developed alongside every new set of guidelines, whether for concussion or some other sports injury, is a clearly defined implementation plan to ensure that the guidelines can actually be adopted readily across all levels and contexts of sporting participation.
My Utopic dream? Guidelines that really make a difference because they can be readily understood and adopted universally.
thanks for those comments caroline, very insightful. in my conversations with drs. leslie and craton (soon to be posted as a podcast) they indicated that one of their greatest concerns relates to the ‘community-level’: both athlete and clinician. that is, the non elite athlete who has a concussion-like injury, sees his GP, who then is following excellent care by attending to the current ‘gold standard’ guidelines for managing such an injury…..and then winds up months later continuing to emphasize cognitive and physical rest in someone whose PCSS is still never getting to zero. the authors argued strongly that, just as you phrased it, the guidelines need to “…really made a a difference because they can be readily understood and adopted universally.” thanks again for writing, i continue to enjoy your twitter posts.
Thanks for your comments. We agree that the adoption of clinical guidelines is a challenging area. We believe that the scenario of a weekend warrior being assessed by a clinician with limited experience in the assessment and management of concussion is well served by the Zurich guideline document. The high sensitivity of the current inclusion criteria insure that patients with potential brain injuries are not allowed to continue in sport, and protected from significant consequences in the acute setting. It is the subsequent management that is problematic, as only a subset of patient’s diagnosed with concussion will actually have a brain injury. The institution of treatment that promotes patient isolation and limited communication has the potential to exacerbate underlying, well documented psycho-social risk factors for the development of prolonged post concussion syndrome reporting. The slide into the morass of post concussion syndrome is one of the eventualities we hope to prevent by the editorial.
Pingback: CJSM Podcast 1 | Clinical Journal of Sport Medicine Blog
Pingback: What to do about concussions? | Clinical Journal of Sport Medicine Blog